Introduction
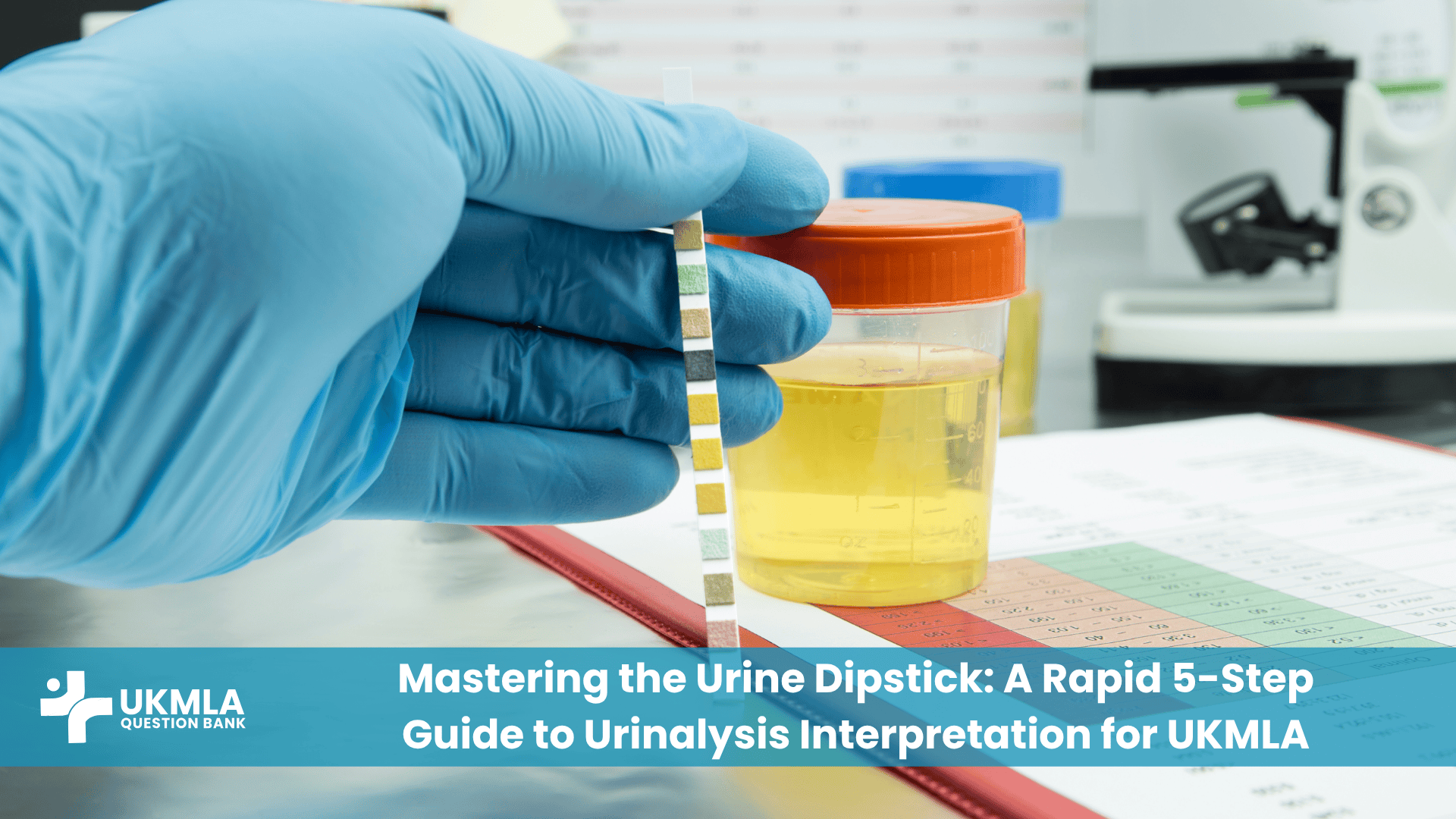
Proficiency in urine dipstick interpretation UKMLA candidates must demonstrate is a cornerstone of basic clinical assessment. This simple, rapid bedside test provides a wealth of information about a patient’s urinary tract, renal function, and metabolic state. From diagnosing a common urinary tract infection (UTI) to flagging potential kidney disease or diabetes complications, the humble urine dipstick is a powerful tool in your diagnostic arsenal.
As a junior doctor, you’ll perform and interpret countless urine dipsticks. This guide provides a clear, 5-step framework to ensure you approach urinalysis systematically and confidently extract the maximum clinical information. We’ll cover correct technique, interpretation of key findings, common pitfalls, and how these results integrate into the broader clinical picture for UKMLA scenarios. For context on where urinalysis fits within broader laboratory testing, see The Ultimate Guide to UK Blood Tests and Lab Values for the UKMLA.
Table of Contents
ToggleKey Takeaways
Technique Matters: Accurate results depend on correct sample collection (mid-stream urine), dipstick handling (brief immersion, correct timing), and comparison with the colour chart.
Leukocytes + Nitrites = UTI: The combination of positive leukocyte esterase and nitrites is highly suggestive of a urinary tract infection (UTI), especially with relevant symptoms.
Haematuria Needs Investigation: Blood in the urine (visible or non-visible) always warrants further investigation to rule out significant pathology (e.g., stones, infection, malignancy), though benign causes exist.
Proteinuria is a Renal Red Flag: Persistent proteinuria, especially when accompanied by haematuria or other signs, requires investigation for kidney disease (e.g., glomerulonephritis, diabetic nephropathy).
Interpret in Context: Like all tests, the dipstick must be interpreted alongside the patient’s clinical presentation, other investigations (e.g., microscopy, culture), and potential interfering factors.
Why Urine Dipstick Interpretation is a Fundamental UKMLA Skill
Urinalysis is a ubiquitous test in clinical practice, featuring frequently in both parts of the UKMLA exam.
The AKT Context: Diagnosing Common Presentations (UTI, AKI)
In the Applied Knowledge Test (AKT), you will likely encounter scenarios involving urine dipstick results. For example, a question might describe a patient with dysuria and provide dipstick findings (positive leukocytes and nitrites), asking for the most likely diagnosis (UTI) or initial management. Other questions might test your understanding of proteinuria as a sign of kidney disease or glycosuria in diabetes.
The CPSA Context: Bedside Testing and Explaining Results
The Clinical and Professional Skills Assessment (CPSA) directly tests your practical skills. You might be required to:
Perform the test: Demonstrate the correct technique for performing a urine dipstick test on a simulated sample.
Interpret results: Be shown a dipstick result and asked to interpret it in the context of a clinical scenario.
Explain findings: Communicate the significance of results (e.g., blood or protein in the urine) to a simulated patient clearly and empathetically.
Formulate a plan: Use the dipstick result to guide further investigations (e.g., sending urine for microscopy, culture, and sensitivity – MC&S) or management.
Performing the Test Correctly: Technique & Common Errors
Garbage in, garbage out. An incorrectly performed test yields unreliable results.
Sample Collection (MSU Essentials)
Ideal Sample: Mid-stream urine (MSU) collected in a sterile container.
Instructions for Patient:
Wash hands thoroughly.
Clean the genital area (women separate labia, men retract foreskin).
Start urinating into the toilet for a few seconds.
Then, collect the middle part of the urine stream into the sterile pot (without stopping urination).
Finish urinating into the toilet.
Replace the lid securely, avoiding touching the inside of the pot or lid.
Wash hands again.
Timing: Test the sample promptly (ideally within 1-2 hours) or refrigerate if delay is unavoidable, as cells degrade and bacteria multiply at room temperature.
Dipstick Handling and Timing
Check Expiry Date: Expired strips give false results.
Brief Immersion: Dip the strip briefly (1-2 seconds) into the urine, ensuring all pads are wetted. Do not soak.
Remove Excess Urine: Tap the edge of the strip against the container rim or blot gently on tissue paper to prevent colours running between pads.
Correct Timing: Read each pad at the specific time indicated on the bottle (usually 30-120 seconds). Reading too early or too late leads to inaccurate colour interpretation.
Good Lighting: Compare the strip colours against the chart on the bottle in good lighting.
Common Errors: Incorrect sample collection (contamination), prolonged immersion, incorrect timing of reading, using expired strips.
The Rapid 5-Step Guide to Urine Dipstick Interpretation UKMLA
Approach the strip systematically. While the order isn’t critical, grouping related tests helps.
Step 1: Visual Inspection (Colour, Clarity)
Before dipping: Look at the urine itself.
Colour: Normal is pale yellow to amber. Dark urine? (Dehydration, bilirubin). Red/brown? (Blood, myoglobin, drugs, beetroot).
Clarity: Normal is clear. Cloudy? (Infection – pus/WBCs, phosphates, contamination).
Step 2: Check for Infection Markers (Leukocytes, Nitrites)
Leukocyte Esterase: Detects an enzyme released by white blood cells (pyuria). Indicates inflammation, usually infection.
Nitrites: Detects nitrite, formed when common urinary tract bacteria (like E. coli) convert nitrates to nitrites. Requires urine to be in the bladder for several hours (often negative in first morning void or frequent urination).
Interpretation: Positive Leukocytes + Positive Nitrites = High likelihood of UTI. Positive Leukocytes alone = Possible UTI or other inflammation. Positive Nitrites alone = Suggestive of UTI (specific but not sensitive).
Step 3: Check for Blood (Haematuria)
Detects: Haemoglobin (from intact or lysed red blood cells) or myoglobin.
Interpretation: Positive result indicates haematuria (or myoglobinuria). Can range from trace to +++. Needs further investigation (microscopy to confirm RBCs, further imaging/tests depending on context).
False Positives: Menstrual contamination, vigorous exercise.
Step 4: Check for Protein & Glucose (Renal & Metabolic Clues)
Protein: Detects albumin primarily. Trace protein can be normal, especially in concentrated urine.
Interpretation: Persistent proteinuria (usually ≥1+) is a significant sign of kidney disease (glomerular damage, diabetic nephropathy) or pre-eclampsia in pregnancy. Requires quantification (ACR/PCR).
Glucose: Detects glucose. Normally absent in urine.
Interpretation: Glycosuria usually indicates hyperglycaemia (blood glucose exceeding the renal threshold, ~10 mmol/L), strongly suggesting diabetes mellitus.
Step 5: Check pH, Ketones, Bilirubin/Urobilinogen & Specific Gravity
pH: Normal range ~4.5-8.0. High pH can suggest UTI (urea-splitting organisms like Proteus). Low pH can occur in acidosis or with certain diets.
Ketones: Normally absent. Presence (ketonuria) indicates fat metabolism due to lack of carbohydrates/insulin. Seen in DKA, starvation, prolonged vomiting, low-carb diets.
Bilirubin/Urobilinogen: Bilirubin normally absent; its presence suggests conjugated hyperbilirubinaemia (liver disease, biliary obstruction). Urobilinogen presence is normal; absence suggests biliary obstruction, while increased levels can indicate haemolysis or liver disease.
Specific Gravity (SG): Measures urine concentration/density. High SG = concentrated urine (dehydration). Low SG = dilute urine (high fluid intake, diabetes insipidus, chronic kidney disease).
Deep Dive: Interpreting Key Findings
Let’s explore the clinical significance of the most important positive results in urine dipstick interpretation UKMLA scenarios.
Leukocyte Esterase & Nitrites: Diagnosing UTI
Mechanism: Leukocyte esterase signifies white blood cells (pus) fighting infection. Nitrites signify the presence of common Gram-negative bacteria converting nitrate.
Significance: Together, they have a high positive predictive value for UTI in symptomatic patients. However, absence doesn’t completely rule out UTI, especially if symptoms are strong or the organism doesn’t produce nitrites (e.g., Staphylococcus saprophyticus).
Next Steps: In a typical adult female with clear symptoms and positive dipstick, empirical antibiotics may be appropriate. In complex cases (male, pregnant, recurrent, catheterised, systemic signs), send urine for Microscopy, Culture & Sensitivity (MC&S). For more context, see Infectious Disease Essentials for UKMLA.
Haematuria: Differential Diagnosis (From UTI to Malignancy)
Significance: Always requires consideration, even if trace. Can be Visible (VH) or Non-Visible (NVH – previously microscopic).
Causes (Simplified):
Infection: UTI/Pyelonephritis (common, often with leukocytes/nitrites).
Stones: Renal or bladder calculi (often with pain).
Malignancy: Bladder, Renal, Prostate Cancer (especially painless VH in older adults – red flag!).
Glomerulonephritis: Kidney inflammation (often with proteinuria, casts on microscopy).
Trauma: Including catheterisation.
Benign: Exercise-induced, menstruation.
Next Steps: Confirm with microscopy (presence of RBCs). Investigate based on clinical picture: MSU for culture, renal function (U&Es, eGFR), imaging (USS/CT KUB), potentially cystoscopy or nephrology referral. Further details are in Nephrology & Urology Essentials for UKMLA.
Proteinuria: Significance and Causes (Including Pre-eclampsia)
Significance: Persistent proteinuria is a key marker of kidney damage. Trace amounts can be transient/benign (e.g., after exercise, fever, postural proteinuria).
Causes:
Glomerular Disease: Glomerulonephritis, diabetic nephropathy (very common).
Tubulointerstitial Disease: Hypertension, drug toxicity.
Overflow: Multiple myeloma (Bence Jones proteins – not detected well by dipstick).
Pre-eclampsia: New onset proteinuria and hypertension after 20 weeks gestation – an obstetric emergency! (See Obstetrics & Gynaecology Essentials for UKMLA).
Next Steps: Repeat test to confirm persistence. Quantify with urine Albumin:Creatinine Ratio (ACR) or Protein:Creatinine Ratio (PCR). Investigate underlying cause (renal function, BP, HbA1c, immunology screen, renal USS).
Glucose & Ketones: Diabetes Red Flags
Glycosuria Significance: Indicates blood glucose has exceeded the kidney’s reabsorption threshold (~10 mmol/L). Strong indicator of undiagnosed or poorly controlled Diabetes Mellitus.
Ketonuria Significance: Indicates significant fat burning for energy. High-yield associations:
Diabetic Ketoacidosis (DKA): Ketones + Glycosuria + Acidosis (low pH if ABG done). See DKA vs. HHS Guide.
Starvation/Prolonged Vomiting: Using fat stores for energy.
Low Carbohydrate Diets.
Next Steps: If glycosuria +/- ketones present, check capillary blood glucose immediately. Further investigations for diabetes (HbA1c) or cause of ketosis are needed.
Bilirubin & Urobilinogen: Clues to Liver Disease
Bilirubin: Should not be in urine. Presence indicates conjugated hyperbilirubinaemia, suggesting biliary obstruction (e.g., gallstones in CBD, pancreatic head tumour) or hepatocellular disease. Urine appears dark.
Urobilinogen: Normally present in small amounts (formed from bilirubin breakdown in gut, reabsorbed). Absence suggests complete biliary obstruction (no bilirubin reaching gut). Increased levels suggest increased bilirubin production (haemolysis) or inability of liver to process it (liver disease).
Table 1: Interpreting Common Urine Dipstick Results
| Parameter | Significance if Positive/Abnormal | Common Causes / Associations |
|---|---|---|
| Leukocyte Esterase | Pyuria (WBCs in urine) | UTI, other inflammation (e.g., stones, tumour) |
| Nitrites | Presence of nitrite-reducing bacteria | UTI (esp. E. coli, Klebsiella, Proteus) |
| Blood (Haem) | Haematuria or Myoglobinuria | UTI, Stones, Malignancy, Glomerulonephritis, Trauma, Rhabdomyolysis (myoglobin) |
| Protein (Albumin) | Proteinuria (persistent is significant) | kidney disease (Diabetic Nephropathy, Glomerulonephritis, Hypertension), Pre-eclampsia |
| Glucose | Glycosuria | Diabetes Mellitus (blood glucose > renal threshold ~10mmol/L) |
| Ketones | Ketonuria | DKA, Starvation, Vomiting, Low-carb diet |
Integrating Dipstick Results with Microscopy & Culture
The dipstick is a screening test. Urine Microscopy, Culture, and Sensitivity (MC&S) provides definitive information:
Microscopy: Quantifies White Blood Cells (WBCs), Red Blood Cells (RBCs), looks for casts (suggestive of renal disease), crystals, and bacteria. Confirms haematuria/pyuria seen on dipstick.
Culture: Identifies the specific bacterial species causing infection (if any).
Sensitivity: Determines which antibiotics the bacteria are sensitive or resistant to, guiding targeted treatment.
When to send MC&S: Suspected UTI with negative/equivocal dipstick, complicated UTI (male, pregnant, catheter, pyelonephritis), recurrent UTIs, persistent haematuria/proteinuria, suspected kidney disease.
Putting It All Together: 3 UKMLA-Style Clinical Scenarios
Case 1: The Young Woman with Dysuria and Frequency
Vignette: A 24-year-old woman presents with a 2-day history of burning pain on urination (dysuria), needing to urinate frequently, and suprapubic discomfort. She feels otherwise well.
Dipstick Results: Leukocytes ++, Nitrites +, Blood Trace, Protein Neg, Glucose Neg.
Interpretation: Positive leukocytes and nitrites strongly suggest a UTI. Trace blood is common with UTI inflammation.
Action: Likely uncomplicated lower UTI. Consider empirical antibiotics as per local guidelines. Advise safety netting. Send MSU for MC&S if symptoms atypical, recurrent, or don’t resolve.
CPSA Sample Script: Explaining UTI Result
“Okay Sarah, thanks for providing that sample. Looking at the dipstick test, it shows signs of inflammation and bacteria in your urine – we call this leukocytes and nitrites being positive. Combined with the burning and frequency you’ve described, this makes a urinary tract infection, or UTI, the most likely cause. I’d like to prescribe a short course of antibiotics which should clear it up quickly. We’ll also send the sample to the lab just to confirm and make sure we’re using the right antibiotic.”
Case 2: The Elderly Man with Painless Visible Haematuria
Vignette: A 70-year-old man presents after noticing blood in his urine today. He has no pain or other urinary symptoms. He is a lifelong smoker.
Dipstick Results: Blood +++, Leukocytes Neg, Nitrites Neg, Protein Trace, Glucose Neg.
Interpretation: Significant haematuria. Trace protein may be related or insignificant. No signs of infection.
Diagnosis & Action: Painless visible haematuria in this demographic is a red flag for urological malignancy (e.g., bladder cancer) until proven otherwise. Urgent (2-week wait) referral to Urology is required for investigation (cystoscopy, upper tract imaging – usually CT urogram).
Case 3: The Pregnant Woman with High Blood Pressure
Vignette: A 30-year-old woman, 32 weeks pregnant in her first pregnancy, attends her routine antenatal check. Her blood pressure is noted to be 150/95 mmHg (previously normal). She reports mild headaches and slight ankle swelling.
Dipstick Results: Protein ++, Blood Neg, Leukocytes Neg, Nitrites Neg, Glucose Neg.
Interpretation: Significant proteinuria (++) in the context of new-onset hypertension in the third trimester.
Diagnosis & Action: This is highly suspicious for Pre-eclampsia. Urgent referral to the obstetric team/maternity assessment unit is required for further assessment (quantification of proteinuria, blood tests including FBC, U&Es, LFTs, Urate), monitoring, and management plan.
Table 2: Causes of Haematuria (Simplified)
| Common Causes of Haematuria | |
|---|---|
| Category | Examples |
| Infection / Inflammation | UTI, Pyelonephritis, Prostatitis, Urethritis |
| Stones (Calculi) | Kidney stones, Bladder stones |
| Malignancy | Bladder Cancer, Renal Cell Carcinoma, Prostate Cancer, Upper Tract TCC |
| Renal (Glomerular) | IgA Nephropathy, Post-infectious Glomerulonephritis, Thin Basement Membrane Disease, Alport Syndrome |
| Structural / Other | Benign Prostatic Hyperplasia (BPH), Polycystic Kidney Disease, Trauma (inc. catheter), Anticoagulants, Exercise, Menstruation |
Frequently Asked Questions (FAQ) about Urine Dipstick Interpretation
A urine dipstick is a highly suggestive screening tool, especially if both leukocyte esterase and nitrites are positive in a symptomatic patient. However, it’s not definitive proof. The gold standard diagnosis requires a positive urine culture (MC&S) demonstrating significant bacteriuria. Clinical correlation is key; treat based on strong suspicion in uncomplicated cases, but always consider MC&S if the picture is unclear, symptoms are severe, or the patient is in a high-risk group (e.g., male, pregnant, recurrent infections).
The dipstick test detects the haem component of haemoglobin or myoglobin. False positives can occur due to menstrual contamination (very common, always ask female patients about their cycle), dehydration causing highly concentrated urine, vigorous exercise (transient haematuria/myoglobinuria), or the presence of oxidising cleaning agents contaminating the sample pot. Myoglobinuria (e.g., from rhabdomyolysis) will also be positive but microscopy will show no red blood cells.
Nitrites are produced when bacteria convert dietary nitrates. A false negative can happen if the urine hasn’t been in the bladder long enough for this conversion (e.g., <4 hours, common with urinary frequency), if the patient’s diet is low in nitrates, or if the infecting organism doesn’t produce the necessary reductase enzyme (e.g., Staphylococcus saprophyticus, Enterococcus, Pseudomonas). Therefore, a negative nitrite test doesn’t rule out a UTI if leukocytes are positive and symptoms are present.
No, trace proteinuria can be physiological, especially in concentrated urine samples (check specific gravity), after strenuous exercise, during fever, or sometimes transiently when standing up (orthostatic/postural proteinuria, usually in young adults). Persistent proteinuria (present on repeat testing, ideally on an early morning sample) at a level of 1+ or higher is considered significant and warrants quantification with a urine ACR or PCR to investigate for underlying kidney disease.
Specific gravity measures the density or concentration of the urine compared to pure water (which has an SG of 1.000). A normal range is typically 1.005 to 1.030. A high SG (>1.030) indicates concentrated urine, often due to dehydration or conditions like SIADH. A consistently low SG (<1.005) indicates dilute urine, which could be due to high fluid intake, diuretic use, diabetes insipidus, or an inability of the kidneys to concentrate urine (seen in chronic kidney disease).
No, not necessarily. In straightforward cases like a first presentation of uncomplicated lower UTI in an adult, non-pregnant female with typical symptoms and a positive dipstick (leukocytes +/- nitrites), empirical treatment according to local guidelines is often appropriate without MC&S. However, MC&S is generally recommended for: suspected pyelonephritis, complicated UTIs (e.g., male patients, pregnancy, catheter-associated, recurrent infections, known renal tract abnormalities), failed initial treatment, or when dipstick results are equivocal but symptoms persist.
Yes, dehydration leads to more concentrated urine (high specific gravity). This can cause physiologically normal amounts of substances like protein or blood cells to appear as ‘trace’ or ‘1+’ positive simply due to the lower volume of water. Always interpret trace results in the context of the specific gravity and the patient’s hydration status. Repeating the test on an early morning sample or after rehydration can be helpful.
Bence Jones proteins are monoclonal immunoglobulin light chains produced in excess by plasma cells in conditions like Multiple Myeloma. They can cause kidney damage (cast nephropathy). Standard urine dipsticks primarily detect albumin and are generally insensitive to Bence Jones proteins. If myeloma or overflow proteinuria is suspected (e.g., unexplained AKI, bone pain, high calcium), specific urine electrophoresis or serum free light chain assays are required; a negative dipstick for protein does not rule out significant Bence Jones proteinuria.
Bilirubin in the urine (bilirubinuria) indicates the presence of conjugated bilirubin, which is water-soluble. This only occurs when there’s liver disease impairing excretion into bile or biliary obstruction preventing bile flow. Unconjugated bilirubin (e.g., from haemolysis) is bound to albumin and doesn’t filter into urine. Urobilinogen is formed in the gut from bilirubin, partially reabsorbed, and normally excreted in small amounts in urine. Increased urobilinogen suggests increased bilirubin production (haemolysis) or reduced liver clearance. Absent urobilinogen suggests complete biliary obstruction.
Yes, several medications can interfere. For example, high doses of Vitamin C (ascorbic acid) can cause false negatives for glucose and blood pads. Some antibiotics (like rifampicin or nitrofurantoin) can discolour the urine orange or brown, potentially interfering with colour interpretation. Phenazopyridine (a urinary analgesic) causes bright orange urine and can interfere with multiple pads (especially nitrite). Always consider the patient’s medication list when interpreting unexpected results.
Conclusion
The urine dipstick is a simple yet powerful diagnostic aid. Mastering urine dipstick interpretation UKMLA style requires combining technical proficiency with systematic analysis and clinical correlation. Using the 5-step approach (Visual, Infection, Blood, Protein/Glucose, Others) ensures you cover the key areas efficiently. Remember the crucial associations – leukocytes/nitrites for UTI, blood as a red flag needing investigation, protein signalling kidney issues, and glucose/ketones hinting at diabetes.
Always perform the test correctly and interpret the results within the full clinical context. Use resources like Lab Tests Online UK for detailed explanations and Patient.info for communication practice. Consistent practice will make urinalysis interpretation a rapid, reliable, and high-yield skill in your clinical toolkit.
Your Next Steps
Practice Perfect Technique: Observe and practice the correct MSU collection and dipstick testing procedure until it’s second nature. Pay attention to timing!
Use the 5-Step System: Consciously apply the framework every time you interpret a dipstick, linking findings (e.g., proteinuria) to relevant knowledge (Nephrology Essentials).
Learn Red Flags: Focus on recognising urgent findings like significant haematuria, proteinuria in pregnancy, or ketones/glucose suggestive of DKA (DKA vs HHS Guide).
Know When to Escalate: Understand when a dipstick result necessitates further action, such as sending an MSU for MC&S or referring for specialist investigation.